HIPAA Questions and Answers: A Comprehensive Guide (Updated December 21‚ 2025)

Navigating HIPAA regulations requires understanding patient rights‚ covered entities‚ and data protection; comprehensive guides and manuals are essential for compliance‚ especially with evolving technology.
Resources from HHS.gov offer official guidance‚ while enforcement actions demonstrate the increasing scrutiny of HIPAA violations‚ impacting healthcare practices significantly.
Staying updated on these regulations‚ including telehealth and messaging app risks‚ is crucial for maintaining patient privacy and avoiding substantial penalties.

What is HIPAA and Why Does it Matter?
The Health Insurance Portability and Accountability Act (HIPAA)‚ enacted in 1996‚ establishes national standards to protect sensitive patient health information. It’s more than just a set of rules; it’s a cornerstone of patient trust within the healthcare system.
Why does HIPAA matter? Primarily‚ it safeguards individual medical records and ensures confidentiality. This protection extends to healthcare providers‚ insurance companies‚ and any entity handling Protected Health Information (PHI). A breach can lead to identity theft‚ discrimination‚ and embarrassment for patients.
Furthermore‚ HIPAA promotes efficiency in healthcare administration by standardizing electronic health records and transactions. Compliance isn’t merely about avoiding penalties – though those can be substantial – it’s about upholding ethical obligations and fostering a secure environment for patient care. Understanding HIPAA is vital for anyone involved in healthcare‚ from doctors to administrators and IT professionals.
The Core Components of HIPAA: Privacy Rule
The HIPAA Privacy Rule centers on protecting individuals’ medical records and other Personally Identifiable Information (PII). It dictates how “covered entities” – healthcare providers‚ health plans‚ and healthcare clearinghouses – can use and disclose PHI.
Key provisions include granting patients the right to access their records‚ request amendments‚ and receive an accounting of disclosures. Covered entities must implement safeguards to protect PHI‚ limiting access to those with a legitimate “need to know.”
Notice of Privacy Practices is a crucial element‚ informing patients about their rights and how their information will be used. The rule also addresses minimum necessary standards‚ ensuring only the minimum amount of PHI is disclosed for a specific purpose. Compliance requires robust policies‚ training‚ and ongoing monitoring.
The Core Components of HIPAA: Security Rule
The HIPAA Security Rule focuses on protecting electronic Protected Health Information (ePHI). Unlike the Privacy Rule‚ it’s specifically geared towards the confidentiality‚ integrity‚ and availability of electronic data.
Three main safeguards are outlined: Administrative‚ Physical‚ and Technical. Administrative safeguards involve security management processes‚ workforce training‚ and risk assessments. Physical safeguards address access control to facilities and devices containing ePHI.
Technical safeguards encompass encryption‚ access controls‚ and audit trails to protect data during transmission and storage. Regular security assessments and updates are vital. The rule is flexible‚ allowing covered entities to tailor safeguards based on their size‚ complexity‚ and risk analysis‚ ensuring a layered security approach.
The Core Components of HIPAA: Breach Notification Rule
The HIPAA Breach Notification Rule mandates specific actions when unsecured Protected Health Information (PHI) is compromised. It establishes national standards for disclosing breaches‚ ensuring individuals are informed about potential misuse of their health data.
A breach generally requires notification to affected individuals‚ the Department of Health and Human Services (HHS)‚ and‚ in some cases‚ the media. The rule outlines a risk assessment process to determine if a breach necessitates notification‚ considering the nature and extent of the compromised information.
Timely notification is crucial; breaches affecting 500 or more individuals require notification within 60 days of discovery. Smaller breaches have varying deadlines. Proper breach response planning and documentation are essential for compliance and mitigating potential penalties.

Frequently Asked Questions About HIPAA Compliance
Addressing common inquiries about HIPAA clarifies obligations for covered entities‚ patient rights‚ and data security; detailed FAQs and guides promote understanding.
Understanding who must comply‚ what information is protected‚ and how to report violations are key aspects of maintaining ongoing HIPAA adherence.
Who Must Comply with HIPAA? (Covered Entities)
HIPAA compliance isn’t universal; it specifically targets “covered entities.” These primarily include healthcare providers – encompassing hospitals‚ clinics‚ physicians‚ and other healthcare practitioners delivering medical care. Health plans‚ such as insurance companies‚ HMOs‚ and Medicare‚ also fall under HIPAA’s purview‚ as they handle protected health information (PHI).
Furthermore‚ healthcare clearinghouses‚ which process nonstandard health information into standard formats‚ are obligated to adhere to HIPAA regulations. Business associates‚ entities performing functions involving PHI on behalf of covered entities – like billing companies or IT support – are also directly accountable.
Crucially‚ understanding this categorization is vital. Organizations not fitting these definitions generally aren’t directly subject to HIPAA‚ though state laws may impose similar privacy obligations. Determining your entity’s status is the first step toward ensuring appropriate compliance measures are implemented and maintained.
What Information is Protected Under HIPAA? (Protected Health Information ౼ PHI)
Protected Health Information (PHI) is the cornerstone of HIPAA’s safeguards. It encompasses any individually identifiable health information relating to a patient’s past‚ present‚ or future physical or mental health condition. This includes medical records‚ diagnoses‚ treatment information‚ and billing details.
PHI extends beyond clinical data; it incorporates demographic information like names‚ addresses‚ birthdates‚ and social security numbers when linked to health information. Importantly‚ even seemingly innocuous data can become PHI if it could potentially identify an individual.
The HIPAA Privacy Rule meticulously defines 18 identifiers that‚ when combined with health information‚ constitute PHI. Understanding this broad definition is critical for covered entities to appropriately protect patient data and avoid potential violations‚ ensuring confidentiality and security.
Patient Rights Under HIPAA

HIPAA grants patients significant control over their health information. Key rights include the right to access their medical records‚ request amendments to inaccurate information‚ and receive an accounting of disclosures – a record of who has accessed their PHI.
Patients also have the right to request restrictions on how their information is used and disclosed‚ and to receive communications via preferred methods and locations. A crucial right is the ability to request a copy of the healthcare provider’s Notice of Privacy Practices‚ detailing how PHI is handled.
These rights empower individuals to actively participate in managing their healthcare data‚ fostering transparency and accountability within the healthcare system. Understanding these rights is vital for patients to protect their privacy and ensure responsible data handling.
Can Family Members Access a Patient’s Health Information?
Generally‚ HIPAA protects patient privacy‚ meaning healthcare providers cannot disclose PHI to family members without explicit patient authorization. However‚ exceptions exist. If a patient is incapacitated or unable to make decisions‚ providers may share information with family involved in their care‚ based on professional judgment.
A patient’s guide clarifies when communication with family is permissible‚ even without authorization‚ focusing on the patient’s best interest. Providers must exercise caution and consider the patient’s prior wishes when making these decisions.
Obtaining valid authorization forms from the patient is the safest approach. These forms specify what information can be shared‚ with whom‚ and for how long‚ ensuring compliance and respecting patient autonomy.
HIPAA and Technology
Modern healthcare relies on technology‚ demanding robust security for electronic health records (EHRs) and telehealth; APIs must adhere to HIPAA guidelines for data protection.
Messaging apps like WhatsApp pose risks‚ requiring careful consideration of privacy and compliance when transmitting protected health information (PHI) digitally.
HIPAA Compliance and Electronic Health Records (EHRs)
Electronic Health Records (EHRs) present unique challenges and opportunities for HIPAA compliance. Covered entities utilizing EHR systems must implement robust administrative‚ physical‚ and technical safeguards to protect Protected Health Information (PHI).
These safeguards include access controls‚ audit trails‚ and encryption‚ ensuring data integrity and confidentiality. Regular risk assessments are crucial to identify vulnerabilities and maintain compliance.
Furthermore‚ EHR systems must support patient rights‚ such as access to their records and amendment requests. Proper training for all personnel handling EHRs is paramount‚ emphasizing HIPAA regulations and security protocols.
Compliance isn’t merely about technology; it’s a holistic approach encompassing policies‚ procedures‚ and ongoing monitoring to safeguard patient data within the digital landscape. Utilizing a HIPAA security manual can greatly assist in this process.
HIPAA and Telehealth: Specific Considerations
Telehealth expands healthcare access but introduces specific HIPAA considerations. Ensuring the confidentiality‚ integrity‚ and availability of PHI during virtual consultations is paramount. Utilizing secure‚ HIPAA-compliant video conferencing platforms is essential‚ avoiding public or unsecured options.
Business Associate Agreements (BAAs) with telehealth providers are crucial‚ outlining their responsibilities for protecting PHI. Providers must also inform patients about the privacy risks associated with telehealth and obtain their consent.
Secure messaging portals and encryption of data in transit are vital safeguards. Risk assessments should specifically address the vulnerabilities inherent in telehealth technologies.
A patient’s guide to HIPAA privacy rules should be readily available‚ clarifying communication protocols with family or involved parties. Maintaining compliance requires diligent attention to these unique challenges.
Using WhatsApp and Other Messaging Apps: HIPAA Risks
Generally‚ using unencrypted messaging apps like WhatsApp for PHI transmission poses significant HIPAA risks. These platforms often lack the necessary security controls and Business Associate Agreements (BAAs) required for HIPAA compliance.
While WhatsApp offers end-to-end encryption‚ it doesn’t guarantee HIPAA compliance due to data storage policies and potential access by the provider. The use of QR codes for linking devices introduces further vulnerabilities if not managed securely.
Healthcare providers should avoid discussing patient information on these apps‚ even seemingly innocuous details. Secure alternatives‚ like HIPAA-compliant messaging platforms‚ are strongly recommended.
A comprehensive HIPAA manual should explicitly prohibit the use of non-compliant messaging apps. Prioritizing secure communication channels is vital for protecting patient privacy and avoiding potential penalties.

HIPAA Violations and Enforcement

Recent enforcement actions highlight increasing scrutiny of HIPAA breaches; penalties can be substantial‚ emphasizing the need for robust compliance programs and detailed security manuals.
What are the Penalties for HIPAA Violations?
HIPAA violations carry tiered penalties based on the level of negligence and intent. Unknowing violations can result in fines ranging from $137 to $68‚928 per violation‚ with an annual maximum of $1.5 million.
However‚ reasonable cause violations escalate fines to $1‚370 to $68‚928 per violation‚ still capped at $1.5 million annually. Intentional neglect‚ where a covered entity knowingly violates HIPAA with malicious intent‚ faces the most severe penalties.
These can reach $68‚928 per violation‚ with no annual limit‚ potentially leading to crippling financial consequences. Beyond financial penalties‚ criminal charges are possible for knowingly obtaining or disclosing protected health information (PHI) under false pretenses‚ carrying potential jail time.
Furthermore‚ reputational damage and loss of patient trust are significant‚ non-monetary consequences of a HIPAA breach‚ impacting long-term viability.
Recent HIPAA Enforcement Actions & Trends (2023-2025)
The Department of Health and Human Services Office for Civil Rights (OCR) has demonstrably increased HIPAA enforcement since 2023‚ focusing on breaches stemming from inadequate security protocols and improper PHI disclosures.
Recent actions highlight settlements with healthcare providers and business associates for failing to implement sufficient safeguards‚ leading to unauthorized access to patient data. A notable trend involves telehealth-related breaches‚ emphasizing the need for secure communication platforms.
Investigations frequently reveal deficiencies in risk assessments‚ employee training‚ and breach notification procedures. OCR is also scrutinizing the use of messaging apps like WhatsApp‚ finding them often non-compliant with HIPAA standards.
Looking ahead to 2025‚ expect continued emphasis on ransomware attacks and the protection of patient data in the face of evolving cyber threats‚ demanding proactive compliance measures.
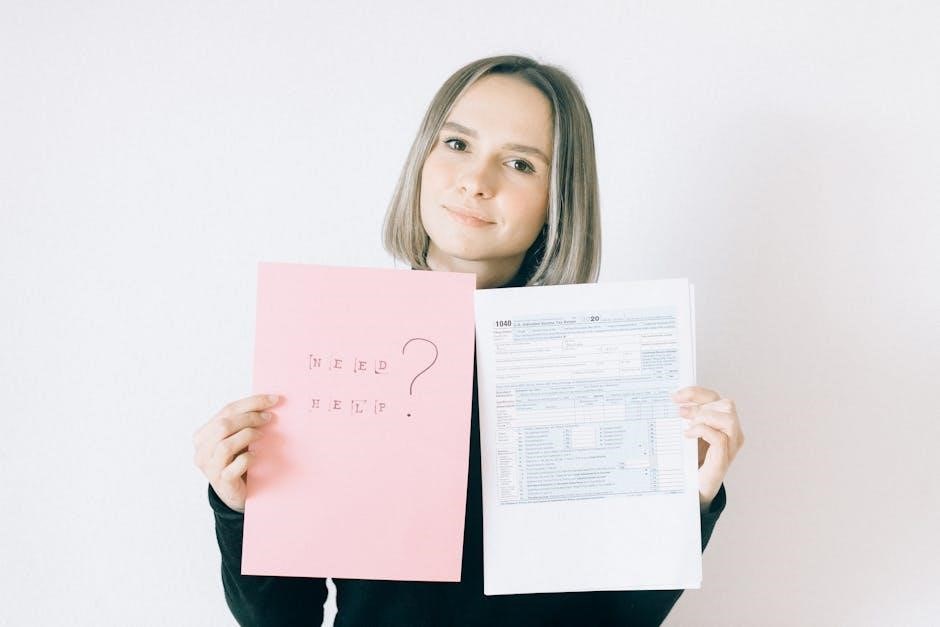
How to Report a HIPAA Violation
Individuals suspecting a HIPAA violation can file a complaint with the Office for Civil Rights (OCR) at the Department of Health and Human Services (HHS). This can be done online through the HHS website‚ offering a streamlined submission process.
Complaints must be filed within 180 days of discovering the violation‚ detailing the covered entity involved‚ the nature of the breach‚ and any harm experienced. Anonymous complaints are accepted‚ though providing contact information facilitates investigation.
The OCR investigates all credible complaints‚ potentially leading to audits and enforcement actions against non-compliant entities. Reporting internally to the organization is also advisable‚ but doesn’t replace filing with OCR.
Furthermore‚ state Attorneys General may also have jurisdiction over HIPAA violations‚ offering an additional avenue for reporting depending on the specifics of the case and location.
Resources and Further Information
HHS.gov provides official HIPAA guidance‚ while specialized manuals aid medical practices; continuous learning ensures ongoing compliance with evolving regulations and enforcement trends.
Where to Find Official HIPAA Guidance (HHS.gov)
The U.S. Department of Health and Human Services (HHS) website‚ specifically the Office for Civil Rights (OCR) section‚ serves as the primary source for official HIPAA guidance. Here‚ you’ll find detailed explanations of the Privacy Rule‚ Security Rule‚ and Breach Notification Rule‚ alongside frequently updated FAQs addressing common compliance questions.
HHS.gov offers access to regulatory text‚ proposed rule changes‚ and final rulings‚ allowing stakeholders to stay abreast of the latest developments. Furthermore‚ the site provides resources on HIPAA enforcement actions‚ offering valuable insights into potential violations and associated penalties.
For those seeking a deeper understanding‚ HHS publishes various toolkits and educational materials designed for covered entities and business associates. These resources simplify complex regulations and provide practical guidance for implementation. Accessing these official materials is crucial for establishing a robust HIPAA compliance program.
HIPAA Manuals and Guides for Medical Practices
Numerous commercially available HIPAA manuals and guides cater specifically to medical practices‚ offering tailored compliance solutions. These resources often include customizable policies and procedures‚ risk assessment templates‚ and staff training materials‚ streamlining the implementation process.
A well-structured manual should cover all core HIPAA components – Privacy‚ Security‚ and Breach Notification – and address specific practice workflows. Look for guides that are regularly updated to reflect the latest regulatory changes and enforcement trends. The Accountability Act (HIPAA) Security Manual is a popular choice.
Selecting a manual should consider practice size‚ specialty‚ and the complexity of its operations. Some guides offer online access and ongoing support‚ ensuring continuous compliance. Remember‚ a manual is a tool‚ and its effectiveness relies on consistent implementation and staff training.
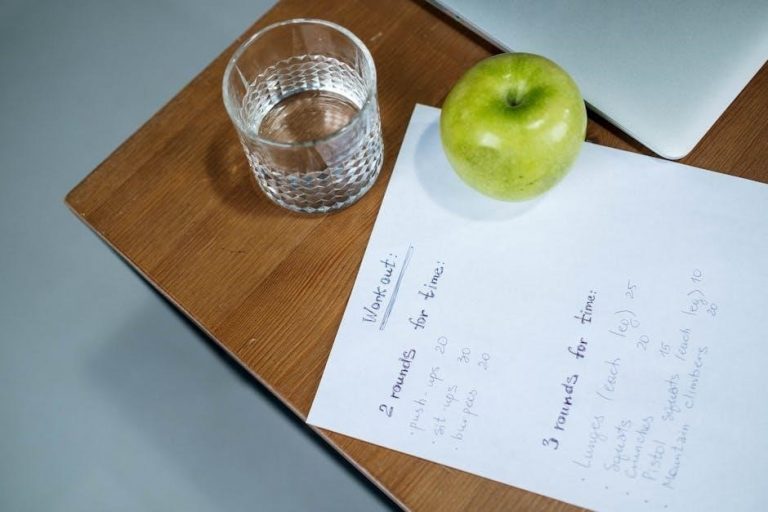
Staying Updated on HIPAA Regulations: Ongoing Compliance
HIPAA compliance isn’t a one-time achievement; it demands continuous monitoring and adaptation. Regulations evolve‚ and enforcement priorities shift‚ necessitating ongoing education and policy reviews. Regularly check the Department of Health and Human Services (HHS) website (HHS.gov) for updates‚ guidance‚ and newly released enforcement actions.

Subscribe to industry newsletters and participate in webinars to stay informed about emerging threats and best practices. Annual staff training is crucial‚ reinforcing HIPAA principles and addressing new challenges‚ like telehealth and mobile device security.
Proactive risk assessments should be conducted periodically to identify vulnerabilities and implement corrective measures. Document all compliance efforts‚ including training records and policy updates‚ to demonstrate due diligence in the event of an audit or breach.