Counseling intake interviews are foundational to building a therapeutic alliance, and often utilize standardized questions found in PDF formats.
These initial sessions establish crucial rapport, gathering essential client information for effective treatment planning and ongoing support.
A well-structured intake process, often documented with forms, ensures a comprehensive understanding of the client’s needs and history.
Professionals leverage these interviews to determine appropriate interventions and navigate the therapeutic journey collaboratively.
The Purpose of Intake Interviews
Intake interviews serve a multifaceted purpose within the therapeutic process, initiating a collaborative journey guided by carefully considered questions, often available as PDF resources.
Primarily, they establish a foundational client-therapist relationship built on trust and open communication, crucial for successful therapy.
These interviews systematically gather comprehensive information – demographics, presenting problems, history – forming a holistic client profile.
This detailed assessment informs diagnostic impressions, treatment planning, and goal setting, ensuring interventions are tailored to individual needs.
Furthermore, intake processes identify potential risks, such as suicidal ideation or self-harm, prompting immediate safety assessments and interventions.
They also clarify administrative aspects like confidentiality, informed consent, and financial arrangements, ensuring transparency and ethical practice.
Ultimately, the intake interview lays the groundwork for a productive therapeutic alliance, maximizing the potential for positive client outcomes.
Standardized questions in PDF format help ensure consistency and thoroughness.
Importance of a Comprehensive Intake
A comprehensive intake is paramount in counseling, utilizing detailed questions – frequently found in readily accessible PDF formats – to establish a strong therapeutic foundation.
It minimizes the risk of misdiagnosis by gathering a complete picture of the client’s history, experiences, and current challenges.
Thorough assessments facilitate the development of individualized treatment plans, maximizing the effectiveness of interventions.
A detailed intake proactively identifies potential safety concerns, like suicidal or homicidal ideation, enabling timely intervention and risk management.
It strengthens the therapeutic alliance by demonstrating the therapist’s commitment to understanding the client’s unique circumstances.
Comprehensive documentation, guided by structured questions, ensures legal and ethical compliance, protecting both client and therapist.
Utilizing standardized PDF intake forms promotes consistency and thoroughness across cases, improving the quality of care.
Ultimately, a robust intake process sets the stage for successful therapeutic outcomes.

Essential Information to Gather
Essential client data, often collected via PDF intake questions, includes demographics, presenting problems, history, and risk factors for effective care.
Client Demographics and Contact Information
Gathering accurate demographic and contact details is the initial step, frequently facilitated by a standardized counseling intake interview questions PDF.
This typically includes the client’s full name, date of birth, address, phone number, and email address, ensuring reliable communication.
Professionals also inquire about gender identity, ethnicity, and preferred pronouns, fostering inclusivity and culturally sensitive care.
Emergency contact information is crucial, including the name and relationship of a trusted individual, alongside their contact details.
Verification of insurance information, if applicable, streamlines the billing process and clarifies coverage details.
Documenting this foundational data establishes a clear record and facilitates efficient administrative procedures throughout the therapeutic process.
These details, often pre-populated on intake forms, save valuable session time and ensure completeness.
Maintaining confidentiality of this information is paramount, adhering to ethical guidelines and legal regulations.
Presenting Problem & Initial Concerns
Exploring the presenting problem is central to the counseling intake interview, often guided by a structured questions PDF.
Clients are encouraged to articulate what brings them to therapy, detailing the specific issues causing distress or impairment.
Open-ended questions like “What brings you here today?” or “What are your primary concerns?” facilitate detailed responses.
The therapist assesses the duration, intensity, and frequency of these concerns, gaining a clearer understanding of their impact.
Exploring the client’s perspective on the problem’s origins and contributing factors is also essential.
Understanding the client’s goals for therapy – what they hope to achieve – provides direction for treatment planning.
Initial assessments also cover the client’s coping mechanisms and previous attempts to address the issue.
This section establishes a collaborative framework, ensuring the therapist and client are aligned on the core issues.
Mental Health History
A thorough mental health history is crucial during the counseling intake interview, often utilizing a detailed questions PDF.
Clinicians inquire about any previous diagnoses, symptoms experienced, and the age of onset for mental health concerns.

Questions explore past hospitalizations, outpatient treatment, and the effectiveness of previous interventions.
Gathering information about family history of mental illness helps identify potential genetic predispositions or patterns.
The intake process assesses current symptoms, including mood, anxiety, sleep disturbances, and changes in appetite.
Exploring the client’s perception of their mental health and any stigma they may experience is also important.
Documentation includes details about any self-harm behaviors or suicidal ideation, requiring careful assessment.
This comprehensive history informs diagnosis, treatment planning, and risk management strategies.
Previous Therapy Experiences
Exploring previous therapy experiences is a vital component of the counseling intake interview, often guided by specific questions in a PDF format.
Clinicians ask about the types of therapy previously tried – individual, group, family – and the client’s reasons for seeking help at that time.
Questions focus on the client’s perception of the effectiveness of past therapy, including what was helpful and unhelpful.
Understanding the therapeutic relationship with previous therapists, including any ruptures or positive connections, is key.
The intake assesses the client’s adherence to previous treatment plans and any barriers encountered.
Exploring the client’s expectations of therapy and any preconceived notions is also important.
Documentation includes the names of previous therapists, dates of treatment, and presenting problems addressed.
This information informs current treatment planning and helps avoid repeating ineffective approaches.
Psychiatric Diagnoses & Medications
Gathering information regarding psychiatric diagnoses and current medications is a critical aspect of the counseling intake interview, often detailed in PDF intake forms.
Direct questions are asked about any previous or current diagnoses received from mental health professionals.
Clients are asked to list all current medications, including dosage, frequency, and prescribing physician.
The intake explores the client’s understanding of their diagnoses and any associated symptoms.
It’s important to inquire about medication adherence, side effects experienced, and any previous medication trials.
Clinicians assess the client’s beliefs about medication and its role in their treatment.
Documentation includes the date of diagnosis, the clinician who provided it, and a complete medication list.
This information informs treatment planning and facilitates collaboration with other healthcare providers.
Substance Use History
A thorough exploration of substance use history is vital during the counseling intake interview, frequently guided by standardized questions within PDF intake forms.
Clinicians inquire about the client’s past and present use of alcohol, tobacco, and illicit drugs.
Specific questions address the frequency, quantity, and duration of substance use.
The intake assesses any previous attempts to quit or reduce substance use, and associated challenges.
It’s crucial to explore any history of substance use disorders, treatment received, and relapse experiences.
Questions also cover the impact of substance use on the client’s life, including relationships, work, and legal issues.
Documentation includes details about substances used, patterns of use, and any related medical or psychiatric complications.
This information informs assessment, treatment planning, and referral to specialized services if needed.

Medical History
Gathering a comprehensive medical history is a critical component of the counseling intake interview, often facilitated by detailed questions in PDF intake forms.
Clinicians inquire about current and past medical conditions, including chronic illnesses, surgeries, and hospitalizations.
Specific questions address current medications, dosages, and any known allergies or adverse reactions.
The intake assesses any physical symptoms that may be contributing to the client’s emotional or psychological distress.
It’s important to explore any history of neurological conditions, head injuries, or chronic pain.
Questions also cover family medical history, particularly regarding mental health or substance use disorders.
Documentation includes details about diagnoses, treatments received, and any limitations in physical functioning.
This information informs assessment, treatment planning, and collaboration with other healthcare professionals if necessary.

Exploring Client Background
Counseling intake interview questions, often in PDF format, delve into a client’s history to understand their developmental journey and current context.
This exploration builds rapport and informs effective treatment.
Family History & Relationships
Family history and relationships are critical components explored during counseling intake interviews, frequently guided by PDF-based questionnaires.
These questions aim to understand the client’s familial dynamics, including the quality of relationships with parents, siblings, and other significant family members.
Therapists inquire about family communication patterns, conflict resolution styles, and any history of mental health issues or substance use within the family.
Exploring early childhood experiences and attachment styles provides valuable insight into the client’s current relational patterns.
Intake forms often ask about significant family events, such as loss, trauma, or major life transitions, and their impact on the client.
Understanding the client’s role within the family system helps identify potential sources of support or stress.
The goal is to gain a comprehensive understanding of the client’s family background and its influence on their emotional well-being.
Social Support System
Assessing a client’s social support system is a vital part of counseling intake interviews, often facilitated using structured questions found in PDF formats.
Therapists explore the client’s relationships with friends, colleagues, and community members to gauge the availability of emotional, practical, and informational support.
Intake forms typically ask about the quantity and quality of these relationships, identifying individuals the client turns to during times of stress.
Understanding the client’s level of social connectedness helps determine their resilience and coping mechanisms.
Questions may delve into the client’s participation in social activities, hobbies, and community organizations.
Exploring any experiences of social isolation or loneliness is crucial for identifying potential areas for intervention.
A strong social support network can significantly contribute to a client’s overall well-being and therapeutic progress.
Trauma History
Exploring trauma history during counseling intake interviews is a sensitive yet crucial component, often guided by carefully worded questions available in PDF formats.
Therapists approach this topic with empathy and respect, recognizing the potential for re-traumatization.
Intake forms may inquire about experiences of abuse, neglect, violence, or other distressing events.
Questions are typically open-ended, allowing clients to share their experiences at their own pace and in their own words.
It’s important to assess the impact of trauma on the client’s current functioning, including emotional regulation, relationships, and self-perception.
Clinicians also explore coping mechanisms developed in response to trauma, both adaptive and maladaptive.
Understanding a client’s trauma history informs treatment planning and ensures trauma-informed care is provided.
Assessment of Risk
Risk assessment during counseling intake interviews, often utilizing PDF-based questions, is paramount for client safety and ethical practice.

Evaluating potential harm to self or others guides immediate intervention and treatment planning.
Suicidal Ideation & Attempts
Assessing suicidal ideation is a critical component of the counseling intake interview, frequently guided by standardized questions available in PDF formats.
Directly inquiring about thoughts of death, wishes to die, or specific plans is essential, despite anxieties about potentially increasing risk.
Clinicians should explore the intensity, frequency, and duration of these thoughts, alongside any prior suicidal attempts or gestures.
Intake forms often include questions about hopelessness, feelings of being a burden, and access to lethal means.
It’s vital to assess the client’s intent, plan, and access to resources, documenting responses thoroughly.
Furthermore, exploring protective factors – reasons for living, support systems – provides a more nuanced understanding.
A safety plan, collaboratively developed with the client, can offer immediate strategies for coping with suicidal urges.
Remember, a thorough assessment informs appropriate interventions and ensures client safety.
Homicidal Ideation
Assessing for homicidal ideation during a counseling intake interview is paramount, often utilizing structured questions found in PDF assessment tools.
Directly, yet sensitively, inquire about thoughts of harming others, including specific individuals and potential plans;
Clinicians must explore the intensity, frequency, and triggers associated with these thoughts, documenting responses meticulously.
Intake forms should include questions regarding access to weapons, past violent behaviors, and feelings of anger or rage.
It’s crucial to assess the client’s intent, plan, and identified targets, considering the potential for harm.
Duty to warn/protect laws may apply, requiring reporting to authorities if a credible threat exists.
Exploring protective factors – reasons against acting on these thoughts – provides a more comprehensive understanding.
Safety planning and appropriate interventions are essential to mitigate risk and ensure public safety.
Self-Harm Behaviors
Assessing self-harm during a counseling intake interview is critical, often guided by standardized questions available in PDF format.
Directly, yet compassionately, inquire about any history of self-injurious behaviors, including cutting, burning, or other methods.
Explore the frequency, intensity, and triggers associated with these behaviors, documenting details carefully.
Intake forms should include questions about the intent behind self-harm – is it to punish, regulate emotions, or feel something?
Assess for suicidal intent alongside self-harm, as they often co-occur, and evaluate the level of medical risk.
Understanding the function of self-harm helps tailor appropriate interventions and coping strategies.
Explore any previous attempts to seek help for self-harm and the client’s willingness to engage in treatment.
Develop a safety plan collaboratively, identifying triggers and coping mechanisms to reduce future harm.
Legal and Ethical Considerations
Intake processes, often utilizing PDF forms with consent clauses, must adhere to legal standards and ethical guidelines regarding confidentiality.
Informed consent, outlining limits to privacy, is paramount before initiating therapy or asking sensitive questions.
Confidentiality and Limits to Confidentiality
Confidentiality is a cornerstone of the therapeutic relationship, and counseling intake interview questions, often presented in PDF format, should explicitly address this.
Clients need clear understanding that their disclosed information remains private, fostering trust and open communication.
However, absolute confidentiality isn’t guaranteed; legal and ethical exceptions exist, requiring careful explanation during the intake process.
Mandatory reporting laws necessitate breaching confidentiality when clients disclose harm to themselves or others, or instances of child/elder abuse.
Furthermore, court orders or subpoenas can compel disclosure of records, though therapists advocate for client protection whenever possible.
Intake forms should detail these limitations, ensuring informed consent and minimizing potential misunderstandings.
Discussing these boundaries upfront establishes a transparent and ethically sound therapeutic framework, respecting both client autonomy and legal obligations.
Professionals must document these discussions thoroughly within the client’s record.
Informed Consent
Informed consent is a vital ethical and legal requirement in counseling, frequently addressed through detailed questions within intake forms, often available as a PDF.
This process ensures clients understand the nature of therapy, potential risks and benefits, and their rights throughout treatment.
Intake documentation should clearly outline the therapist’s qualifications, therapeutic approach, and fees associated with services.
Clients must be informed about confidentiality limits, as previously discussed, and the procedures for addressing grievances or concerns.
The consent form should emphasize the voluntary nature of therapy, allowing clients to terminate sessions at any time.
A thorough intake includes a discussion of alternative treatment options, empowering clients to make informed decisions.
Obtaining signed consent demonstrates the client’s understanding and agreement to participate in therapy under the outlined conditions.
Regularly revisiting consent ensures ongoing awareness and client autonomy.

Resources and Further Information
Counseling intake resources, including sample questions and PDF forms, are widely available online from professional organizations and mental health websites.
These tools aid practitioners in creating comprehensive and legally sound intake processes.
Where to Find Sample Intake Forms (PDF)
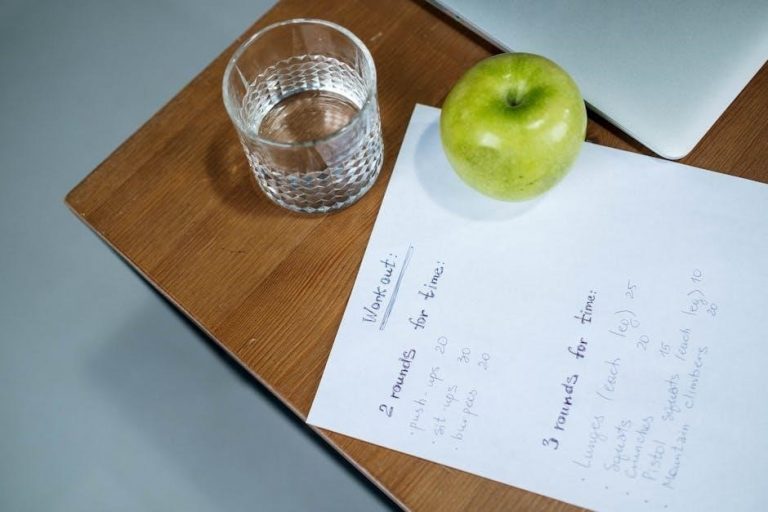
Numerous online resources offer downloadable counseling intake form PDF templates to assist practitioners in gathering essential client information. The American Counseling Association (ACA) often provides resources for members, potentially including sample forms or links to reputable sources.
Websites specializing in practice management software, like SimplePractice or TherapyNotes, frequently offer free intake form templates as part of their service offerings. These PDFs often include sections for demographics, presenting problems, medical history, and consent forms.
Psychology Today’s website and various state psychological associations may also host or link to sample intake questionnaires. A targeted Google search using keywords like “therapy intake form PDF” or “counseling assessment questionnaire” will yield a plethora of options. Remember to review any downloaded form to ensure it aligns with your specific practice needs and legal requirements.
Always prioritize confidentiality and data security when utilizing and storing these forms.